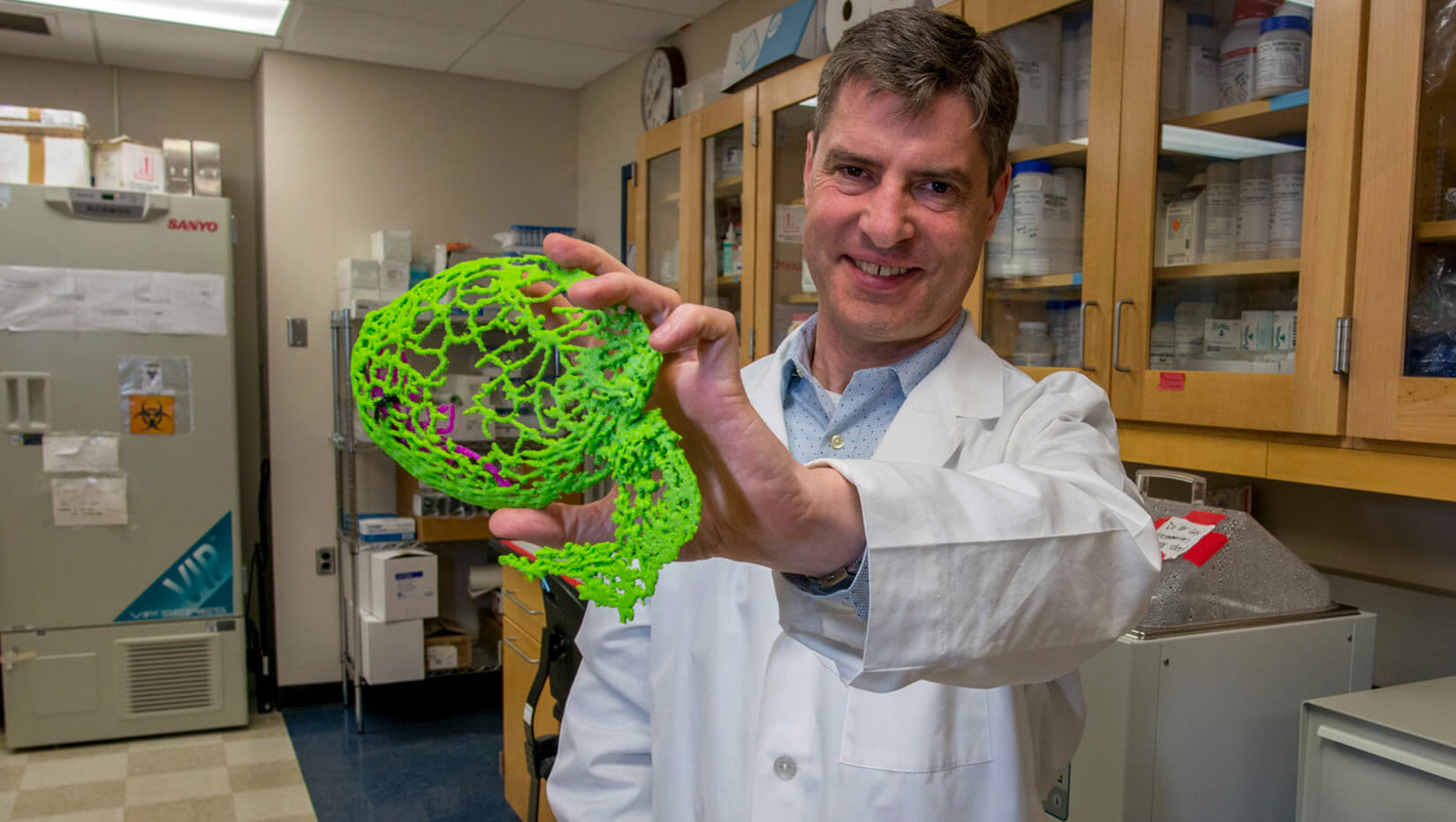
Wheeler probes how potentially lethal fungal infection eludes body’s defenses
Rob Wheeler is engrossed with a generally harmless fungus that naturally lives in and on people, but also can cause disease and death.
For 16 years, the University of Maine associate professor of microbiology has been unraveling the mysteries of the fungus Candida albicans.
The National Institutes of Health recently awarded Wheeler a three-year $428,429 grant to illuminate interactions between C. albicans and the immune system in order to advance treatment and prevention of infectious diseases.
The funding also will support C. albicans research of five graduate students and eight or nine undergraduates in the Wheeler Lab.
This natural gut flora, for the most part (with the exception thrush and vaginal infections), peacefully co-exists in people with healthy immune systems.
But in people whose immune systems are compromised — think transplant patients and people with cancer — this opportunistic fungus gets into the bloodstream and transforms into a potentially fatal, organ-attacking pathogen.
Wheeler explores how neutrophils (white blood cells that lead the immune system’s response to fight infection), the epithelial barrier (the safety shields between internal cells and microbes in the environment), and other innate immune components interact with C. albicans throughout an infection.
He uses zebrafish to watch the interactions. The freshwater fish in the minnow family is nearly transparent in the larval stage, has a similar genetic structure to humans and, like people, is a vertebrate with the same major organs and tissues. Zebrafish and humans also respond to infections and vaccinations in similar ways.
Remi Gratacap, a former postdoctoral fellow in the Wheeler Lab, compares C. albicans to invaders seeking to get past a castle’s multiple defenses — armed guards, walls and a moat.
People, like castles, also have barriers, mechanisms and fighters to hold off pathogens, says Gratacap, who now works at The Roslin Institute at the University of Edinburgh.
For this NIH project, Wheeler will examine how the fungus gets past barriers and into the body’s inner sanctum. And, he says, “We need to understand how the host knows it’s damaged and how it responds.”
Researchers often examine interactions between one infection and the immune system. But multiple pathogens can simultaneously attack people. And Wheeler is interested in understanding how the pathogens interact with each other and the host’s immune systems.
In previous research, scientists in the Wheeler Lab, including former master’s student Audrey Bergeron, discovered that how the fungus C. albicans and the bacteria Pseudomonas aeruginosa interact depends on where they meet.
In healthy people, P. aeruginosa can cause skin rashes and mild ear and eye infections. But in hospital patients with weakened immune symptoms, serious P. aeruginosa infections can lead to severe illness and death.
For a decade, it’s been known that P. aeruginosa attacks and kills C. albicans when they meet in a test tube.
Wheeler and Bergeron, who earned a master’s in biochemistry in May 2017, surmised the same type of antagonistic interaction might occur in a zebrafish swim bladder (similar to a human lung).
They anticipated the bacteria P. aeruginosa again might suppress the C. albicans fungus in the zebrafish and thereby help prevent an infection.
“Boy, were we wrong,” says Wheeler.
Instead, the P. aeruginosa strengthened the virulence of the C. albicans, resulting in more zebrafish deaths than if the zebrafish were singularly infected by C. albicans.
In zebrafish swim bladders — internal mucus-coated gas-filled organs that control buoyancy — they tracked various fungal, bacterial and immune dynamics in real time as well as which fish survived and which died.
Wheeler describes the interaction between the bacteria and fungus as a back-and-forth molecular dialogue that ultimately results in the host being damaged, sometimes fatally.
Observing these interactions in the transparent zebrafish is similar to watching a TV show, with no volume and a surprise ending, Wheeler says.
A next step, say Bergeron and Wheeler, is exploring how, when and why the bacterial-fungal antagonistic crosstalk in a petri dish morphs into an empowering positive interaction in the zebrafish.
That involves developing tools to be able to “listen” to the dialogue and signals, says Wheeler, one of the few people in Maine who studies infectious diseases.
People with lung infections, including those with cystic fibrosis, also sometimes simultaneously fight more than one pathogen.
So Bergeron and Wheeler talked with physicians at Eastern Maine Medical Center who treat patients with the genetic disorder.
In the lungs of people with cystic fibrosis — about 30,000 people in the U.S — mucus builds up and traps germs, which leads to infections and labored breathing. About 80 percent of people with cystic fibrosis eventually die of infection or infection complications.
Wheeler said EMMC physicians are interested in UMaine research that will inform and advance treatment options for patients with cystic fibrosis. For example, would a more effective course of treatment focus on eliminating the bacteria, eliminating the fungus, or both?
Bergeron, who worked as a microbiology analyst at Nephron Pharmaceuticals in South Carolina, now is a research associate at Maine Medical Center Research Institute in Scarborough, Maine.
In August 2017, her paper “Candida albicans and Pseudomonas aeruginosa Interact To Enhance Virulence of Mucosal Infection in Transparent Zebrafish” was published in American Society for Microbiology’s journal Infection and Immunity.
Wheeler, Brittany Seman and Linda Archambault of UMaine and John Hammond and Deborah Hogan of Dartmouth College also participated in the research. The Burroughs Wellcome Fund, the National Institutes of Health and the Department of Agriculture provided funding for the study.
Bergeron’s findings, says Wheeler, built on a previous discovery by Gratacap, the former postdoctoral fellow.
Gratacap had demonstrated that neutrophils control infection by attacking C. albicans and preventing the fungus from invading zebrafish tissue.
His findings were published online in June 2017 in the article “Control of mucosal candidiasis in the zebrafish swimbladder depends on neutrophils that block filament invasion and drive extracellular trap production,” also in American Society for Microbiology’s journal Infection and Immunity. Wheeler, Allison Scherer and Seman took part in the research.
Contact: Beth Staples, 207.581.3777
